In This Article
- What is Serotonin Syndrome?
- What Causes Serotonin Syndrome?
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin-norepinephrine Reuptake Inhibitors (SNRIs)
- Tricyclic Antidepressants (TCAs)
- Monoamine Oxidase Inhibitors (MAOIs)
- Specific Migraine Medication
- ADHD Medications
- Phenylpiperidine Series Opioids
- Morphine and other Opiates
- Illicit Stimulant Drugs
- Psychedelic Drugs
- Symptoms of Serotonin Syndrome
- How Does Serotonin Syndrome Work?
- Can Marijuana Cause Serotonin Syndrome?
- Can I Smoke Weed While Taking Antidepressants?
- Resources
Serotonin is a chemical the body naturally produces. Serotonin is one of the more well-known neurotransmitters because it regulates multiple body processes in the brain, including mood.
THC, the intoxicating compound in cannabis, has been studied in relation to how it affects the way the body metabolizes selective serotonin reuptake inhibitors (SSRIs).1 These medications increase serotonin levels in the body. As such, one of the concerns when using cannabis is: Can weed cause serotonin syndrome?
But what is serotonin syndrome? And can cannabis actually cause it or increase the risk of contracting it?
This article explores the complex relationship between cannabis and serotonin, as well as the risks associated with this serious medical condition.
What is Serotonin Syndrome?
Serotonin syndrome occurs when serotonin levels become too high in the brain. Serotonin is often called the “feel-good hormone” because of its role in regulating mood. Lower levels of serotonin are often linked to depression, while higher levels are often linked to positive emotions.
When serotonin levels get too high, many of the systems that the neurotransmitter regulates get out of balance. This isn’t something that often happens naturally. Instead, serotonin levels are typically altered by medications, many of which boost serotonin levels in order to treat common psychological conditions like depression.
The most common antidepressant medications are selective serotonin reuptake inhibitors (SSRIs). Cannabis has been studied for its potential to interact with SSRIs and other antidepressant medications, like monoamine-oxidase inhibitors (MAOI). Specifically, researchers have questioned how likely it is that cannabis use could increase the risk of serotonin syndrome.
Making things more complicated, side effects after consuming too high a dose of THC can look similar to the effects of serotonin syndrome. It’s often characterized by dilated pupils, stiffness in the lower extremities, and involuntary muscle contractions in the feet.
While THC toxicity, sometimes called “greening out,” isn’t typically considered dangerous, it can still be an uncomfortable or distressing experience for consumers. Serotonin syndrome, on the other hand, is a severe condition that can be life-threatening in extreme cases. If you’re not sure whether you’re experiencing a THC overdose or serotonin syndrome, seek medical attention.
What Causes Serotonin Syndrome?
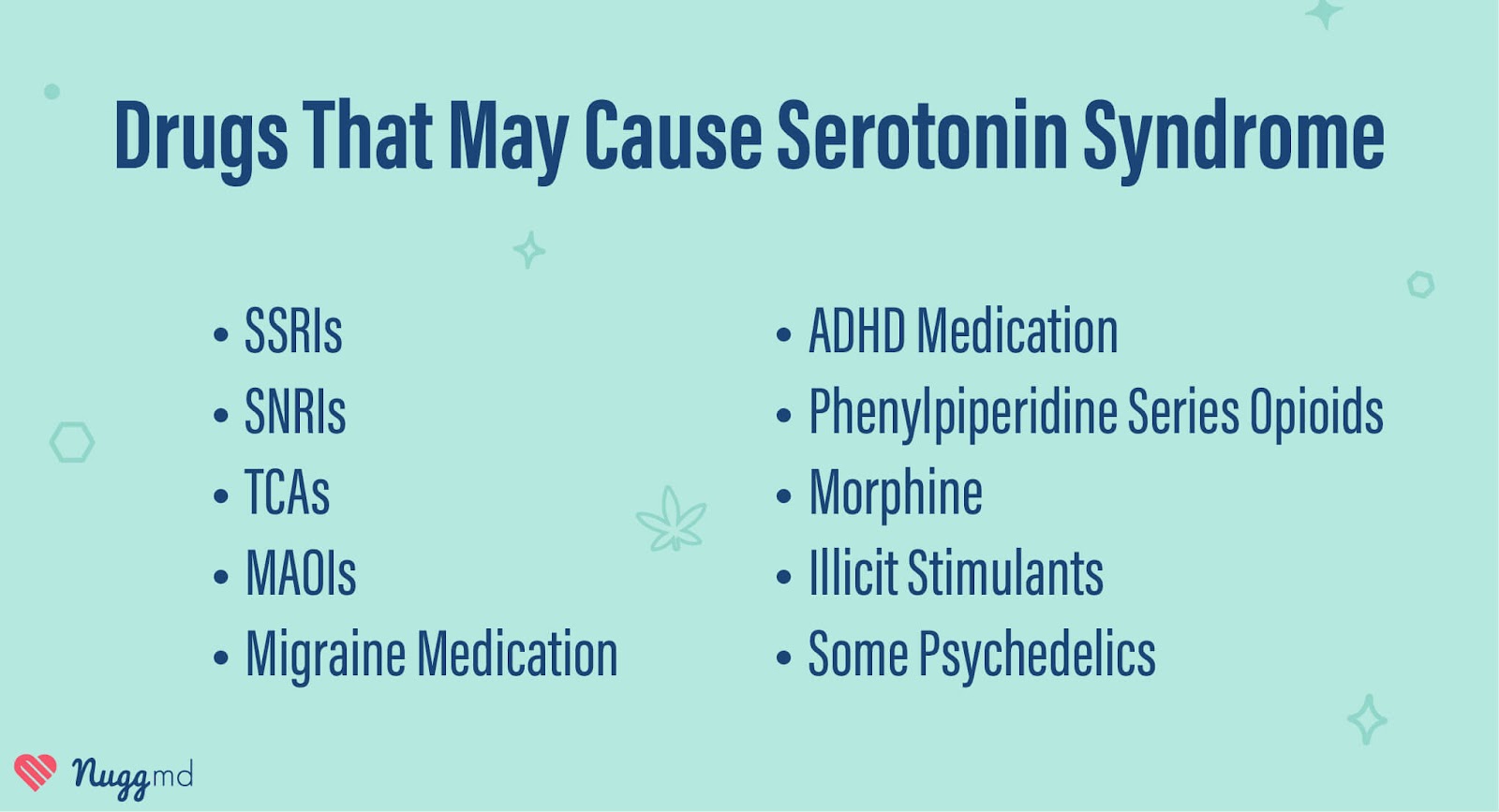
Serotonin syndrome rarely, if ever, happens on its own. It’s usually a reaction caused by drugs that increase serotonin levels in the brain. These drugs are typically types of stimulants or antidepressants prescribed to treat anxiety, depression, and ADHD. However, an increased risk of serotonin syndrome can also occur with medications prescribed for migraines, pain, and other psychological conditions.
Some illicit drugs may also cause serotonin syndrome. For example, MDMA is a common stimulant that’s known for boosting serotonin levels.
While it is highly unlikely that marijuana can cause serotonin syndrome on its own, it can interact with other substances known to increase serotonin levels, changing the way the body processes them and leading to greater risk.
Below are the drug classifications most commonly associated with serotonin syndrome.
Selective Serotonin Reuptake Inhibitors (SSRIs)
SSRIs are a common class of antidepressant medications that work by preventing the body from reabsorbing serotonin, leaving more available for the brain to use. These medications are typically used to treat depression but are often prescribed for other conditions, like OCD.
Common SSRIs include:
Serotonin-norepinephrine Reuptake Inhibitors (SNRIs)
Serotonin-norepinephrine reuptake inhibitors (SNRI) are a class of antidepressant medications that work by stopping the body from reabsorbing serotonin and norepinephrine. This increases the amount of neurotransmitters within the brain that help regulate mood. SNRIs are typically prescribed for depression and anxiety disorders.
Common SNRIs include:
- Desvenlafaxine (Pristiq)
- Duloxetine (Cymbalta)
- Levomilnacipran (Fetzima)
- Venlafaxine (Effexor XR)
Tricyclic Antidepressants (TCAs)
Tricyclic antidepressants (TCA) are among the oldest types of antidepressant medications. They work by blocking the body from reabsorbing serotonin and norepinephrine, and they get their name from the chemical structure of their active ingredients, which typically form three rings.
Unlike more modern antidepressants, TCAs are associated with a wide range of side effects, which is why they’re typically reserved for situations where other antidepressant medications have been ineffective.
Common TCAs include:
- Amitriptyline (Elavil)
- Clomipramine (Anafranil)
- Dosulepin/dothiepin (Prothiaden)
- Imipramine (Tofranil)
- Lofepramine (Gamanil)
- Nortriptyline (Pamelor)
Monoamine Oxidase Inhibitors (MAOIs)
MAOIs work by blocking monoamine oxidase, an enzyme the body uses to remove neurotransmitters, like serotonin, dopamine, and norepinephrine. They can be effective, but they also affect other systems in the body, which could lead to side effects and undesirable interactions with food and other medications. MAOIs have a risk of increasing blood pressure. These medications are most often prescribed when other antidepressants are unsuccessful.
Common MAOIs include:
Specific Migraine Medication
Triptans are a class of migraine medication that works by stimulating serotonin to bind to receptors in the brain, signaling blood vessels to constrict and helping reduce inflammation. These medications act on serotonin in the brain and can potentially lead to serotonin syndrome. Usually, though, any risk of serotonin syndrome from triptans comes from mixing them with another medication.
ADHD Medications
Many medications used to treat ADHD are stimulants that increase levels of several neurotransmitters in the brain, including serotonin. On their own and when used as prescribed, the risk of serotonin syndrome from these medications is minimal. However, when combined with other serotonin-boosting medications, the risk increases.
Common ADHD medications include:
Phenylpiperidine Series Opioids
Phenylpiperidine opioids are a class of medications that bind to opioid receptors in the brain to relieve pain. There is an increased risk of serotonin syndrome in individuals using phenylpiperidine opioids, especially in those who are also taking other medications that boost serotonin levels.
Common phenylpiperidine opioids are:
- Fentanyl (Actiq, Duragesic, Fentora, Sublimaze)
- Methadone (Dolophine, Methadose)
- Meperidine (Demerol)
- Tramadol (Ultram)
Morphine and other Opiates
Morphine and other opiates are commonly used to treat pain. These are powerful medications that carry with them a serious risk of dependence and overdose. While they aren’t usually associated with serotonin syndrome on their own, they are associated with increased serotonin levels when combined with other medications.
Common opiates include:
Illicit Stimulant Drugs
There are a number of illegal stimulant drugs that also affect serotonin levels in the brain. These drugs are best known for the “elevated” sensations they produce. Those sensations are the result of the drugs influencing the brain and its neurotransmitters like serotonin. While these drugs carry other risks, they also amplify the chances of serotonin syndrome, especially when used along with another drug that increases serotonin levels.
Common illicit stimulants include:
- Methylenedioxymethamphetamine (MDMA)
- Amphetamine
- Methamphetamine
Psychedelic Drugs
Psychedelic drugs aren’t the same as stimulants, opiates, or antidepressants, but many psychedelics do interact with serotonin receptors in the brain. The risk of serotonin syndrome from psychedelics is considered very low, but when used with other drugs that increase serotonin levels, there is an increased chance serotonin syndrome can occur.
Common psychedelics include:
- Psilocybin
- Lysergic acid diethylamide (LSD)
- Dimethyltryptamine (DMT)
- Mescaline
Other drugs include Bupropion (Wellbutrin), St. John’s Wort, Lithium, Linezolid, and Ritonavir.
Symptoms of Serotonin Syndrome

The symptoms of serotonin syndrome vary from mild to life-threatening. Mild cases of serotonin syndrome can be hard to diagnose, as even moderate symptoms can be caused by other factors (including THC use). Even moderate symptoms may be caused by other factors, including excessive THC use.
Serotonin syndrome can be dangerous and lead to coma or death if untreated. If you think you may be experiencing serotonin syndrome, it’s always best to be cautious and seek medical attention.
Common symptoms of serotonin syndrome include:
- Agitation or restlessness
- Insomnia
- Confusion
- Rapid heart rate
- High blood pressure
- Dilated pupils
- Loss of coordination
- Muscle twitches
- Muscle rigidity
- Sweating
- Diarrhea
- Headaches
- Shivering
- Goosebumps
In more severe cases, serotonin syndrome can cause:
- High fever
- Tremors
- Seizures
- Irregular heartbeat
- Unconsciousness or coma
- Death
How Does Serotonin Syndrome Work?

Serotonin syndrome is caused by an excess of serotonin in the brain. This rarely occurs naturally and is usually caused by a combination of medications that increase serotonin, either by stopping the brain from absorbing serotonin or by increasing serotonin production.
While it isn’t completely understood, some research indicates that cannabis can impact the way the body metabolizes some antidepressant medications, like SSRIs. Some experts are concerned that this can lead to unexpected increases in serotonin levels and, in rare instances, serotonin syndrome.
Can Marijuana Cause Serotonin Syndrome?
It’s highly unlikely that cannabis alone can cause serotonin syndrome. Cannabis acts on the endocannabinoid system, an entirely different set of receptors throughout the brain and body. However, there is evidence that cannabinoids like CBD and THC can interact with certain medications, like antidepressants and migraine medications, in ways that may increase the risk of serotonin syndrome.
Can I Smoke Weed While Taking Antidepressants?
If you’re planning to use medical cannabis to treat anxiety or depression, speak to your doctor about your current antidepressant medication to limit the risks of an adverse drug interaction.
It’s important to remember that some effects of cannabis can look like symptoms of serotonin syndrome, including drowsiness, dizziness, agitation, and even paranoia. If you’re using cannabis and feel these effects in the short term, it may be a side effect of the cannabis itself. However, if they worsen or persist after cannabis use, or if you have any concerns that the cause could be serotonin syndrome, you should seek medical attention.
Resources
- Vaughn SE, Strawn JR, Poweleit EA, Sarangdhar M, Ramsey LB. The Impact of Marijuana on Antidepressant Treatment in Adolescents: Clinical and Pharmacologic Considerations. J Pers Med. 2021;11(7):615. Published 2021 Jun 29. doi:10.3390/jpm11070615 ↩︎
The information in this article and any included images or charts are for educational purposes only. This information is neither a substitute for, nor does it replace, professional legal advice or medical advice, diagnosis, or treatment. If you have any concerns or questions about laws, regulations, or your health, you should always consult with an attorney, physician or other licensed professional.