Cannabis has a number of reported uses. While many consumers will claim the plant can do no harm, there are specific precautions that cannabis users should take when it comes to combining prescription medications and cannabis. As it turns out, cannabis may interact with prescription antibiotics, which are used to fight off bacterial infections like MRSA, pneumonia, tetanus, E. coli, syphilis, and more.
This article will explore the risks or benefits that may occur when individuals combine their prescription antibiotics with cannabinoids like THC and CBD.
What are Antibiotics?

Antibiotics are a class of drugs used to treat bacterial infections caused by bacteria and parasites. Various antibiotics work through different pharmacological pathways to kill the bacteria that is causing the infection. Depending on what kind of bacteria they treat, these antibiotics can be defined as broad-spectrum or narrow-spectrum. Antibiotics are not used to treat viral infections such as the flu, cold, or COVID-19. To treat viral infections, you must use antiviral medication.
Unfortunately, the overuse of antibiotics can cause the body to develop bacterial infections that are resistant to the current medicines. One example is methicillin-resistant staphylococcus aureus, better known as MRSA (a type of staph infection). This infection is an antibiotic-resistant strain, making it difficult to treat with standard antibiotics.
There are several antibiotic types. The main ones include;
- Penicillins - i.e., phenoxymethylpenicillin, flucloxacillin, and amoxicillin.
- Cephalosporins - i.e., cefaclor, cefadroxil, and cefalexin.
- Tetracyclines - i.e., tetracycline, doxycycline, and lymecycline.
- Aminoglycosides - i.e., gentamicin and tobramycin.
- Macrolides - i.e., erythromycin, azithromycin, and clarithromycin.
- Sulfonamides and trimethoprim - i.e., co-trimoxazole.
- Quinolones - i.e., ciprofloxacin, levofloxacin and norfloxacin.
- Metronidazole and tinidazole.
- Nitrofurantoin.
- Clindamycin.
The most common antibiotics people know about are penicillins, like amoxicillin. However, there are a variety of antibiotic medications that individuals can use to treat a number of bacterial infections. The type of antibiotic a doctor prescribes is determined by the kind of bacteria, the severity of the infection, the patient’s kidney and liver function, potential side effects, and other pertinent medical histories like current medications, if you may be pregnant, and if you have had a reaction to an antibiotic in the past.
What Antibiotics May React with Cannabis?
Certain cannabinoids, like THC and CBD, may affect how effective certain antibiotics are during treatment. In combination with prescription medications, THC has the potential to change how the drug works within the body. Similarly, CBD can alter how the body metabolizes the drug. Research also seems to indicate that CBD presents a higher risk than THC of reacting with antibiotics when combined with other prescription medications. However, the research is in the preliminary stages, and further study needs to be done on the safety profile of combining cannabinoids and antibiotic drugs.
So, what do we know about cannabis and antibiotics?
We know that certain antibiotic drugs, like amoxicillin, tetracycline, erythromycin, and clindamycin, are metabolized through the same CYP450 enzymes as cannabinoids.
CYP450 enzymes are found within the liver and are vital in the breakdown of prescription drugs, as well as cannabinoids, when ingested via edibles or excess sublingual doses. In the case of cannabinoids, these CYP450 enzymes are responsible for the breakdown of delta-9 THC to 11-OH-THC, the more potent metabolite of THC known for providing a stronger and longer-lasting effect than smoking. The cannabinoids, CBD, THC, CBN, and their metabolites, like 11-OH-THC, can act as inhibitors of these CYP450 enzymes, CBD more than 11-OH-THC.
Prescription drugs can also act as CYP450 enzyme inducers or inhibitors. As a result, consuming cannabinoids while taking one of these prescription drugs could cause a change in the metabolism of the prescription drug or alter how the drug works. Because of this interaction with the CYP450 enzymes, the prescription drugs or cannabinoids may become more concentrated in the system, which could reduce the efficacy of the drug or result in increased negative side effects from the medication.
For example, CBD is an inhibitor of the CYP3A4 enzyme, as are tetracycline, erythromycin, ciprofloxacin, and clarithromycin. By inhibiting the CYP3A4 enzyme, the drug concentration can increase, leading to possible toxicity or an increased risk of adverse side effects, including nausea, vomiting, diarrhea, stomach pain, and a lack of appetite.1
One other concern when it comes to taking antibiotics is the inherent risk that comes with smoking. Smoking while on antibiotics – particularly when treating a respiratory, throat, or mouth infection, can interfere with the healing process.
If you’re taking antibiotics for any reason, refraining from smoking cannabis may aid in achieving a speedy recovery!

Find natural, lasting relief with our comprehensive (and completely free) patient’s guide to medical cannabis for chronic pain.
Can Cannabis Help Fight Bacterial Infection?
Many cannabinoids have been studied for their antibiotic effects. In fact, all of the major cannabinoids, such as THC, CBD, CBG, CBN, and CBC, have demonstrated antibacterial properties. Of these cannabinoids, CBG has been shown to have some of the most potent antibacterial properties, as it may help kill MRSA infections. In addition to CBG, the other major cannabinoids, THC, CBD, CBN, CBC, and their acid forms, have also been demonstrated to help fight MRSA infections by killing stationary MRSA cells. For example, CBCA showed a more potent antibacterial effect than vancomycin, a prescription antibiotic, against MRSA.
The endocannabinoid anandamide has also been shown to fight MRSA infections as well, which may provide some more insight into the mechanisms of cannabinoids and why they demonstrate antimicrobial effects. A 2020 study out of Israel found that when combined with ampicillin, anandamide shows strong effectiveness against MRSA infections. In addition to cannabinoids, terpenes such as beta-caryophyllene, myrcene, limonene, and pinene have also been shown to have antibacterial properties against E. coli, staph infections, and more.
These studies on cannabinoids and their antibiotic effects have been mainly limited to in vivo studies, which means they were done on human cell lines infected with things like MRSA and E. coli. Unfortunately, human clinical trials on the antibiotic effects of cannabinoids are still limited.
What About CBD and Antibiotics?
Current research surrounding CBD and antibiotics has indicated that CBD shows neither a synergistic or antagonist effect on MRSA when combined with the following antibiotics: Vancomycin, Methicillin, Clindamycin, Tobramycin, Teicoplanin, Ofloxacin, and Meropenem.
What does that mean?
Essentially, when these antibiotics were used in combination with CBD, they didn’t show an increase or decrease in effectiveness. However, since CBD is an inhibitor of the CYP3A4 enzyme, caution should be taken when taking prescription medications such as tetracycline, erythromycin, ciprofloxacin, and clarithromycin, which also inhibit the CYP34A enzyme.
Does CBD interact with any other antibiotics?
Against general staph infections, CBD has demonstrated an ability to increase the effectiveness of kanamycin. In an infection found in the blood and lungs called Pseudomonas aeruginosa, CBD has been shown to be as effective as the generic antibiotics ciprofloxacin, gentamicin, and ampicillin for fighting the infection. CBD may also enhance the antibiotic vancomycin to fight against E. coli, though further research is required.
With many studies still in the early stages and with so much complexity surrounding the use of antibiotics, consumers would still do well to speak with their doctor before continuing a cannabis regimen while on antibiotics.
When Not to Use Antibiotics with Cannabis
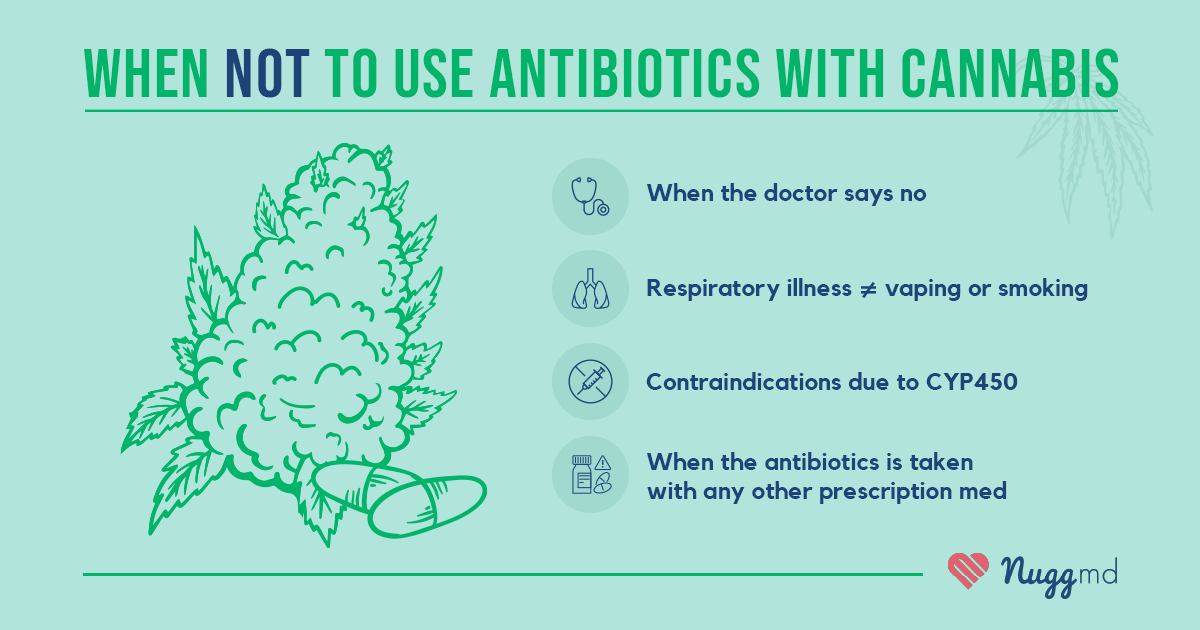
It is always advised to consult with your prescribing physician about the use of cannabis while taking any prescription medication.
Research recommends that individuals allow two or more hours between taking prescription medications and cannabis. Ideally, antibiotics and cannabis use should not be combined under the following conditions:
- When your prescribing physician cautions explicitly against it.
- When the antibiotics are for lung or respiratory infection, and the method of cannabis consumption is smoking or vaping.
- When the medication has contraindications due to its CYP450 metabolism.
- When taking any other prescription medications in combination with prescription antibiotics.
Conclusion
The cannabis plant contains hundreds of compounds, and due to its federal Schedule I status, research remains limited. Because the science is still developing, it is wise to take caution when combining cannabis with your prescription medications.
The current research tells us that cannabinoids and many prescription drugs, like antibiotics, are metabolized through the liver via the CYP450 enzymes. In sharing a common method of metabolization, there is some potential for cannabis use to increase or decrease the concentration and effectiveness of prescription medications.
Overall, more research on the safety and efficacy of combining cannabinoids with prescription antibiotics needs to be done. For now, individuals should consult with their doctor before combining cannabis and prescription medications to determine the safest course of action for their treatment plan.
References
- Lynch T, Price A. The effect of cytochrome P450 metabolism on drug response, interactions, and adverse effects. Am Fam Physician. 2007;76(3):391-396.
- Preissner S. Drug Interactions Involving the Cytochrome P450 Enzymes: Analysis of Common Combinations of Antibiotics and Pain Relieving Drugs. Journal of Drug Metabolism & Toxicology. 2012;03(05). doi:10.4172/2157-7609.1000131
- Feldman M, Smoum R, Mechoulam R, Steinberg D. Potential combinations of endocannabinoid/endocannabinoid-like compounds and antibiotics against methicillin-resistant Staphylococcus aureus. Hegde NR, ed. PLOS ONE. 2020;15(4):e0231583. doi:10.1371/journal.pone.0231583
- Mahmud MS, Hossain MS, Ahmed ATMF, Islam MZ, Sarker ME, Islam MR. Antimicrobial and Antiviral (SARS-CoV-2) Potential of Cannabinoids and Cannabis sativa: A Comprehensive Review. Molecules. 2021;26(23):7216. doi:10.3390/molecules26237216
The information in this article and any included images or charts are for educational purposes only. This information is neither a substitute for, nor does it replace, professional legal advice or medical advice, diagnosis, or treatment. If you have any concerns or questions about laws, regulations, or your health, you should always consult with an attorney, physician or other licensed professional.