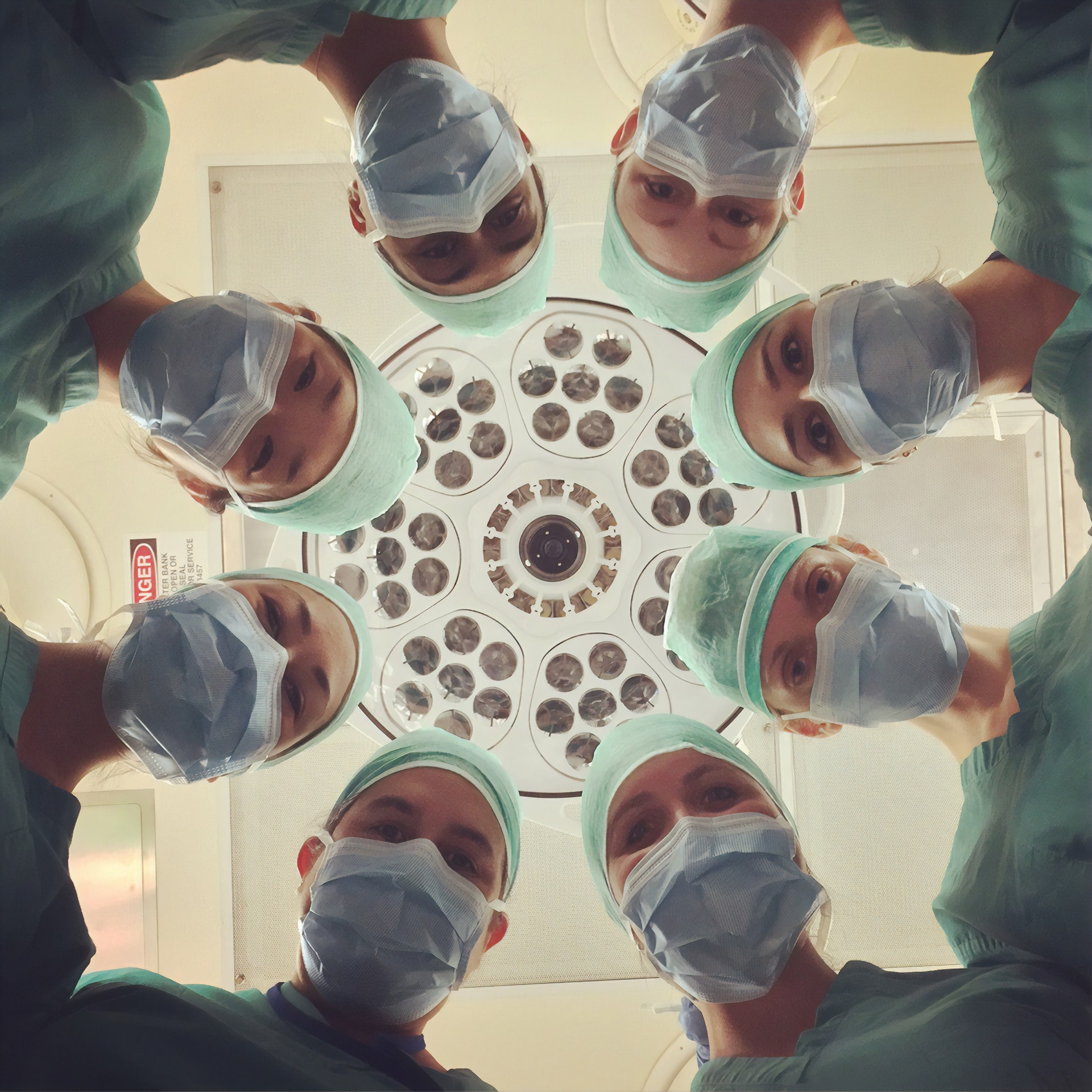
The increasing acceptance of marijuana may pose a new issue: cannabis users who are about to undergo surgery.
Few people know that marijuana use can affect anesthesia and potentially increase complications during surgery. In this article, we discuss how cannabis use can impact a medical operation and what you should do if you are undergoing surgical treatment.
The Relationship Between Weed and Anesthesia
Research on the relationship between weed and anesthesia has long suggested that they are not the friendliest combination. The cannabis plant has an array of compounds anesthesia may interact with during surgery. Disclosing cannabis use to your physician and anesthesiologist is essential to keeping you safe in surgery.
While a patient is under the knife, the anesthesiologist is focused on monitoring your dosage and brain activity. Anesthesiologists use a bispectral index monitor that analyzes the patient's brain activity through an EEG (Electroencephalogram) and produces a number between 0 and 100, called a bispectral index.
This bispectral index indicates how deep your anesthesia is:
- An ideal range is 40 to 60 to prevent the patient from waking up in surgery.
- A bispectral index below 40 indicates lower levels of consciousness,
- while a number over 60 means the individual is more conscious.
Cannabis users have always been considered to have a higher bispectral index during surgery, meaning they would need more anesthesia to stay in the ideal range.
Research has even suggested that elevations in brain wave activity may be caused by cannabinoids, thus making the bispectral index monitor less reliable in determining how deep the anesthesia is due to it being calculated by brain wave activity. Research has also noted that cannabis use can increase the dose required for patient intubation during surgery.
A study from 2018 monitored 27 cannabis users who were undergoing surgery. The patients were put under general anesthesia and given a placebo or a high or low dose of Sativex (1:1 CBD/THC spray) 20 minutes before going under anesthesia. The results showed that the patients who had been given high and low doses of Sativex had a higher bispectral index (BIS) than patients who had been given the placebo. It’s important to note that the study could not determine if these results were related to CBD and anesthesia interaction or THC and anesthesia interaction due to Sativex containing both compounds.1,2
Another study reviewed the medical records of 250 patients who had been sedated and found that those who reported cannabis use needed significantly higher levels of sedation than non-cannabis users. The researchers reported that cannabis users required 14% more fentanyl, 19.6% more midazolam, and 220.5% more propofol than non-users to stay sedated during surgery. It is important to note that this study had a small sample size of cannabis users, having only 25 patients who had reported their use prior to surgery.3
- Alexander JC, Joshi GP. A review of the anesthetic implications of marijuana use. Baylor University Medical Center Proceedings. 2019;32(3):364-371. doi:10.1080/08998280.2019.1603034
- Laudanski K, Wain J. Considerations for Cannabinoids in Perioperative Care by Anesthesiologists. Journal of Clinical Medicine. 2022;11(3):558. doi:10.3390/jcm11030558
- Twardowski MA, Link MM, Twardowski NM. Effects of Cannabis Use on Sedation Requirements for Endoscopic Procedures. The Journal of the American Osteopathic Association. 2019;119(5):307. doi:10.7556/jaoa.2019.052
Why It’s Important to Tell Your Doctors About Cannabis Use
It is always best to disclose your use and be honest with your doctors, as they want to keep you safe. Because cannabis use can cause physiological changes, surgeons and anesthesiologists take preventative measures to reduce the chances of complications during surgery.
Surgeons and anesthesiologists need to determine if the patient is a new or chronic user, when their last use was, are they a medical or recreational user, and how often and in what form they are using cannabis. In determining recent cannabis use, doctors are also ensuring that the patient is coherent enough to consent to the procedure as required by law. Answering these questions truthfully helps your anesthesiologist and doctor determine the best course of action for surgery.
Prior to surgery, patients often have urine and blood samples taken, so the nurses and doctors will be made aware of an individual’s cannabis use. Failing to notify your doctor or anesthesiologist leaves them having to play catch up in the operating room to meet your sedation needs.
To reduce the risk of complications during surgery, doctors and anesthesiologists will generally ask individuals to refrain from using cannabis for at least 72 hours before undergoing surgery. And when operating on cannabis consumers, they may avoid the use of sedative drugs that have been shown to increase the physiological effects of cannabis.
Marijuana and Surgery: Complication Risks
At present, research on cannabis and surgical complications indicates a number of potential risk factors. The most significant complication that can arise when pairing marijuana with surgery is the increased sedative drugs the patient will need to stay unconscious during their surgery. Several studies have noted that higher levels of propofol, the drug often used for general anesthesia, along with fentanyl and midazolam, were necessary for patients who were cannabis users.
Research has suggested that THC can inhibit gastric emptying, which, if you know, having an empty stomach is necessary for surgery. A delay in gastric emptying can result in vomiting while sedated, and it becomes a choking hazard for patients.
Cannabis use also affects an individual's heart rate, which may lead to heart complications such as a fast heartbeat known as tachycardia, a slow heartbeat known as bradycardia, and irregular heartbeats known as arrhythmias. These abnormalities in heart rate during surgery can lead to cardiac arrest and even death.
While often considered a less serious risk of combining cannabis use and surgery, cannabis consumption can also affect body temperature regulation, possibly increasing the risk of hypothermia and shivering after surgery.
Other potential complications that could come with combining marijuana and surgery include:
- Hyperreactive airway - Similar to asthma, your lungs can overreact to an irritant and become swollen; in the case of surgery, the irritant could be the inhalable anesthesia.
- Sinus arrest - An abnormal heart rhythm, causing a pause in activity.
- Hypotension - Low blood pressure.
- Coronary spasms - A tightening of the arteries supplying blood to the heart.
Much of the research notes that the concerns with marijuana and surgery are also time-dependent. Acute physiological effects of cannabis use are typically short-lived but are the most important to consider when undergoing surgery. The more recent the cannabis use (within 72 hours of surgery) the greater risk there is for complications. 1
Risks of Chronic Cannabis Use
Chronic cannabis users also have a higher risk of complications, mainly regarding heart rate and respiratory function. The research for complications in chronic cannabis users seems to indicate that they are more likely to be caused by the act of smoking cannabis rather than the compounds in cannabis. For example, chronic users may be more at risk for experiencing an alveolar hemorrhage, which is when blood floods the air sacks of the lung. An alveolar hemorrhage is a life-threatening risk for patients.
Smoking poses a safety risk to consumers on its own when it comes to undergoing surgery. Smoking can cause blood clots in your legs, reduce healing time, and increase the risk of infection after surgery. Chronic smokers can have more damage to the heart and lungs, which may result in more issues during surgery. For example, smokers have increased levels of Carbon monoxide in their blood, which limits the available oxygen needed for bodily processes, including those keeping your body in balance during surgery.2
However, some studies suggest that chronic cannabis use may not impact surgical outcomes – or may even carry some benefits for patients undergoing surgery.
A 2021 study by Zhang et al. looked at 1152 non-cannabis users and 524 cannabis users who had undergone surgery. The researchers found that there was no statistical significance between marijuana use and surgery or surgical outcomes.4 A separate 2021 study by Yeung et al. found that cannabis users who underwent surgery needed less support for blood pressure monitoring.3
Overall, researchers must conduct more extensive clinical studies to determine the safety of combining marijuana and surgery.
- Echeverria-Villalobos M, Todeschini AB, Stoicea N, Fiorda-Diaz J, Weaver T, Bergese SD. Perioperative care of cannabis users: A comprehensive review of pharmacological and anesthetic considerations. Journal of Clinical Anesthesia. 2019;57:41-49. doi:10.1016/j.jclinane.2019.03.011
- Tønnesen H, Nielsen PR, Lauritzen JB, Møller AM. Smoking and alcohol intervention before surgery: evidence for best practice. British Journal of Anaesthesia. 2009;102(3):297-306. doi:10.1093/bja/aen401
- Yeung BG, Ma MW, Scolaro JA, Nelson AM. Cannabis Exposure Decreases Need for Blood Pressure Support During General Anesthesia in Orthopedic Trauma Surgery. Cannabis Cannabinoid Res. 2022;7(3):328-335. doi:10.1089/can.2021.0009
- Zhang BH, Saud H, Sengupta N, et al. Effect of preoperative cannabis use on perioperative outcomes: a retrospective cohort study. Regional Anesthesia & Pain Medicine. 2021;46(8):rapm-2021-102479. doi:10.1136/rapm-2021-102479
What To Do Before Your Surgery
Individuals who undergo surgery are suggested to disclose the following to their physicians before the procedure:
Cannabis or other drug use
✓ Your doctor should alert the anesthesiologist to your cannabis use so they can monitor their dosing accordingly, but you can also alert the anesthesiologist directly before surgery.
✓ Other recreational drugs like LSD, cocaine, heroin, and ecstasy can also affect the anesthesia and operation and, if used, should be disclosed to your doctor before surgery.
Prescription medication use
✓ Patients should also disclose the use of certain prescriptions like aspirin, warfarin, and more to their doctor.
Any other health conditions, current and prior
✓ Current and prior health conditions such as a heart condition, if you are currently pregnant or breastfeeding, have diabetes, high blood pressure, and more can impact anesthesia and surgical procedures and outcomes.
To help decrease the risk of surgical complications, cannabis users, in particular, should refrain from using cannabis for at least 72 hours before the start of surgery. Patients should also avoid drinking alcohol and smoking cigarettes for at least one week before surgery, as both can interfere with the surgical procedure, anesthesiology, and healing process.
By following the steps outlined above, medical cannabis patients and recreational consumers can help reduce the risk of complications during their surgery. If doctors are unaware of potential confounding variables, they are unable to adjust their procedure to minimize complications. It is always better to be honest with your doctors so they can make informed decisions to keep you safe while under their care.
The information in this article and any included images or charts are for educational purposes only. This information is neither a substitute for, nor does it replace, professional legal advice or medical advice, diagnosis, or treatment. If you have any concerns or questions about laws, regulations, or your health, you should always consult with an attorney, physician or other licensed professional.